Abstract
Background: Patients living with myelodysplastic syndromes (MDS) have significantly worse health-related quality of life (HRQoL) than that of the general population, especially in regards to fatigue, dyspnea, and social functioning. However, there is limited data about the effects of MDS on mental health, and on patients’ social and emotional wellbeing. Furthermore, while caregivers are an integral part of patient care, little is known about how caring for patients with MDS impacts the wellbeing and health of caregivers themselves.
Methods: To better understand the mental health of patients with MDS and the impact of MDS on HRQoL among patients and caregivers, three validated surveys of self-reported outcomes were completed by patients with MDS and their caregivers from May 5 - October 6, 2021. Participants were identified and recruited from the patient database and social media outreach groups of the Aplastic Anemia and MDS International Foundation. Surveys consisted of the PHQ-4, the FACT-An (only FACT-G portion if caregivers), and the Caregiver Self-Assessment (CSA) Questionnaire. Patients with MDS who had already received a bone marrow transplant or who had an additional hematologic condition were excluded from the study. Caregivers with a personal diagnosis of a hematologic condition were excluded. Data were analyzed using means and medians, and comparison between groups was calculated using the chi-square test. A two-sided p value < 0.05 was used to determine significance. Linear regression was used in the FACT surveys, while logistics regression was applied to the results of the PHQ-4 and CSA Questionnaires. Potential confounders including pre-existing mental health diagnoses and performance status were adjusted in the models.
Results: In total, 133 complete patient responses and 25 complete caregiver responses were received. Among patient responders, 52% (n=69) were over 60 years of age, with a mean of 5 years since MDS diagnosis. Approximately 25% (n=36) of patients had self-reported high-risk disease and 44% (n=58) had received at least 1 disease modifying therapy. Among caregiver respondents, 48% (n=12) were over 60 years of age, and 84% (n=21) were female.
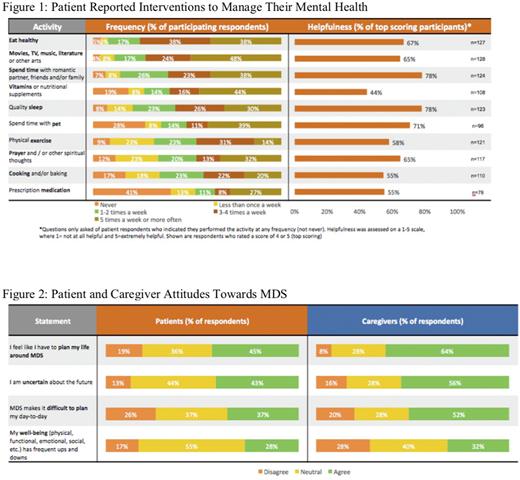
36% (n=58) of MDS patients and caregivers had moderate or severe scores on the PHQ-4, indicating concerning levels of depression and/or anxiety. Functional impairment (p < 0.05), high risk MDS (p < 0.05), and transfusion dependency (p < 0.001) were associated with worse mental health as measured by elevated PHQ-4 scores, whereas good support networks and lack of financial concerns positively impacted mental health (both p < 0.001). MDS patients spent an average of 6 hours at the infusion center to receive a transfusion, and 60% (n=10) of patients required assistance to get to their infusion center, with 30% (n=5) rating their mode of transportation as moderately or considerably difficult. The most common interventions that patients found helpful to manage their mental health are shown in Figure 1.
In certain instances, the burden of MDS was reported to be even more severe by caregivers than patients. Interestingly, as seen in Figure 2, caregivers reported a larger impact of MDS on their lives than patients, particularly in regards to planning and uncertainty about the future. Most caregivers (60%, n=15) reported a high degree of distress as per the Caregiver Self-Assessment Questionnaire. Compared to patients, caregivers reported lower average emotional, social, and functional wellbeing as reported on the FACT survey, but higher physical wellbeing. The COVID pandemic moderately or significantly worsened the mood of a significant proportion of MDS patients (30%, n=40) and caregivers (48%, n=12), especially in regards to worsening social isolation and inaccessibility of resources and travel.
Conclusions: MDS has a significant impact on the mental health of patients and their caregivers, and patients with high-risk disease, functional impairment, or transfusion dependence are at elevated risk for anxiety and depression. The mental health of caregivers also suffers in a manner similar to, and sometimes worse than, patients themselves, suggesting that caregivers could benefit from intervention and outreach from health care professionals as well. Further investigation is needed to identify the helpfulness of specific tools and interventions that may improve mental health and quality of life in this patient population.
Disclosures
Shim:Charles River Associates: Current Employment; Merck / Acceleron: Research Funding; AAMDS Foundation: Research Funding. Backor:Charles River Associates: Current Employment; Merck / Acceleron: Research Funding; AAMDS Foundation: Research Funding. Sloan:Charles River Associates: Current Employment; Merck / Acceleron: Research Funding; AAMDS Foundation: Research Funding. Sweere:Charles River Associates: Ended employment in the past 24 months; Merck / Acceleron: Research Funding; AAMDS Foundation: Research Funding; Teiko.bio: Current Employment. Leblanc:BlueNote: Consultancy; BMS/Celgene: Consultancy, Research Funding, Speakers Bureau; Agios/Servier: Consultancy, Speakers Bureau; Flatiron: Consultancy; BeiGene: Honoraria; Astellas: Consultancy; Genentech: Consultancy; AbbVie: Consultancy, Speakers Bureau; AstraZeneca: Consultancy, Research Funding; GSK: Consultancy; Pfizer: Consultancy.
OffLabel Disclosure:
Growth factors (such as EPO) for MDS
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal